Electronic medical records were not designed with transgender people in mind. Clinicians at the Johns Hopkins Center for Transgender Health are working to change that.
Johns Hopkins Center for Transgender Health: Ever Forward!
by Paula Neira and Devin O’Brien-Coon
In the current political environment, the transgender community faces great challenges to maintain the progress made in addressing basic health care needs such as access to care and insurance coverage. The situation is far from acceptable, but progress because of the Affordable Care Act and changes in Medicare and Medicaid have allowed many transgender individuals to gain insurance coverage for medically necessary care and to be able to see providers for both transgender-health-related care and general health care.
As leaders of the Johns Hopkins Center for Transgender Health (JHCTH), our goal is to address the health care disparities faced by the transgender community. The following are some of the issues about which we are often asked.
Working with patients via the PCORI grant for the EQUALITY Study
The EQUALITY Study was a multi-site, PCORI-funded study that concluded in 2016. The Johns Hopkins Hospital and Howard County General Hospital, along with two sites in Boston, investigated the question of how best to collect sexual orientation and gender identity (SOGI) information from patients in an emergency medicine setting. The phases of the study looked at both the collection methods to capture the data and which staff role (registration or clinicians) was best suited to collect the information. As JHCTH was not established, the Center was not involved directly in the study. However, several key members of the JHCTH team were involved. Our Clinical Program Director, Paula, was a member of the Stakeholder Advisory Board and the nurse champion in the Department of Emergency Medicine for the study. Brandyn Lau, a principle investigator on the study, is a leader of the Center’s team involved in transgender-related research. Dr. Adrian Dobs, a Center champion in endocrinology, and Dr. Tonia Poteat, a leading member of our research team, were also members of the Stakeholder Advisory Board.
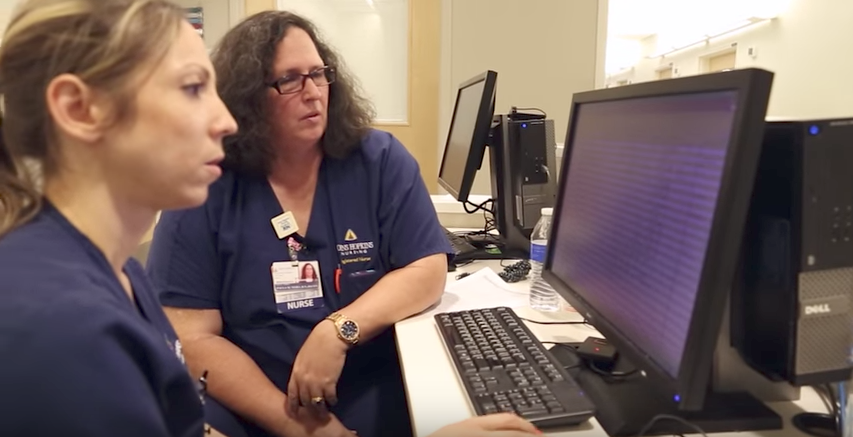
The JHCTH does collect SOGI information as part of our clinical intake process. We believe that this information is vital to being able to deliver supportive, affirming and patient-centered care. Part of establishing the Center, and in collaboration with our Office of Diversity & Inclusion, is providing education and cultural competency training across Johns Hopkins Medicine. A dimension of this education is sharing why this information is important and demonstrating how to ask the questions in an open, professional and welcoming manner. Another dimension is updating the electronic medical records to display the information in a manner that is usable to staff. Remember that electronic medical records were not designed with transgender people in mind and Hopkins clinicians are working to rectify that oversight.

Asking about SOGI has not been part of our culture – at Hopkins or anywhere else in academic medicine – and implementing these demographic questions requires a cultural change that will not happen overnight. Health care organizations and leaders will need to be committed to making the cultural changes and holding staff accountable. One of the first published findings of the EQUALITY study was an article in JAMA Internal Medicine that reported a severe mismatch in perspective. Almost 78% of health care professionals think LGBTQ people do not want to be asked about their sexual orientation whereas 90% of patients would provide the information if asked. Such a difference in perceptions obviates the need for much more health care professional education and increased cultural competency.
Improving health care provider knowledge about trans health
This is not just about physicians. Across the health care disciplines, there has been a lack of education about LGBTQ health needs in general, and about transgender health care needs specifically. Nurses, physicians, advanced practice providers, administrators, and allied health professionals all need to develop cultural competency skills in order to improve the health of the transgender community and reduce the health disparities that transgender patients face. Leaders and educators must ensure that these education needs are included in entry-level academic programs, residency programs, continuing education offerings and all staff orientations.
Transgender health care is but one of many competing clinical priorities in the 21st century. The transgender community needs to recognize in partnering with medical educators there is no room for additional mandatory courses. The pace of new knowledge and breadth of knowledge needed in health care today is overwhelming. Practitioners need to learn more, faster.
It is also not enough simply to create a “Transgender Health care 101” elective. The individuals most likely to need the education are the ones least likely to sign up for such a course. Alternatively, time constraints, regulatory and accreditation requirements (as they currently exist), and lack of faculty, make adding another mandatory course not feasible for many institutions. Creating another online module for existing staff also requires additional time and support because requiring additional education impacts direct patient care by pulling clinicians away from patients. To incorporate transgender health care education across all levels of experience and disciplines effectively, we would identify three fundamental requirements:

- The commitment of leaders across the institution to include the education and provide the resources to produce quality education. Further, to hold staff accountable for developing the cultural competency and employing the skills in
- Infuse transgender health care education across the existing curriculum. Talk about aspects of care in courses where it is already most relevant.
- Encourage accreditation bodies and state regulatory boards to include criteria for licensure and organizational accreditation that addresses cultural competency and knowledge of transgender health. Some jurisdictions, such as the District of Columbia, require continuing education in LGBTQ health for renewing a license. If transgender-related questions appear on the National Council Licensure Examination (NCLEX ), which is the basic entry-level nursing exam, or on a physician specialty-certification board, the material would be included in the coursework.
The creation and mission of the Johns Hopkins Center for Transgender Health
The mission of the Johns Hopkins Center for Transgender Health is to reduce health care disparities and improve the overall health of the transgender community through world-class clinical care, medical education and research. Embracing diversity and inclusion, the Center for Transgender Health provides affirming, objective, person-centered care to improve health and enhance wellness; educates interdisciplinary health care professionals to provide culturally competent, evidence-based care; informs the public on transgender health issues; and advances medical knowledge by conducting biomedical research.

It is our hope that the transgender community will judge our center on the quality of the care we deliver and the manner in which we deliver it. Leadership at Hopkins were very clear in their charge for the creation of this center – we will do it right, we will do it well, and we will do it according to our Core Values and mission.
As we write, we are preparing for the full opening of our Center for Transgender Health. This center is built as an interdisciplinary service line – meaning that providers from all stakeholder services combine to form a team to provide integrated and comprehensive care. We have specialists from primary care, endocrinology, plastic surgery, urology, OB/GYN, fertility preservation, pediatrics, social work, nursing, speech pathology, dermatology, and other allied health providers participating in providing our transgender patients with a world class and respectful patient experience. We will build in partnership with the transgender community and with our colleagues in the health care community.
Change can never happen fast enough for those who are facing discrimination and barriers to care. At Johns Hopkins Medicine, we are committed to moving ever forward to provide great care, teach the next generation of providers, and contribute to increasing our knowledge about transgender health.
About The Authors
 Paula M. Neira JD, MSN, RN, CEN
Paula M. Neira JD, MSN, RN, CEN
Clinical Program Director, Johns Hopkins Center for Transgender Health
Paula M. Neira is a Naval Academy graduate, Desert Storm veteran, nurse, and lawyer. She helped lead the efforts to repeal the Don’t Ask, Don’t Tell policy and is a leading expert on transgender military service. She has specialized in emergency nursing and nursing education in her 20+ year nursing career. Since November 2016, she has been the Clinical Program Director for the Johns Hopkins Center for Transgender Health.
 Devin O’Brien-Coon, MD
Devin O’Brien-Coon, MD
Medical Director, Johns Hopkins Center for Transgender Health
Dr. O’Brien Coon completed his plastic surgery training at the Johns Hopkins University/University of Maryland integrated residency program and gained additional experience in advanced gender-affirming surgery at programs in the United States, Spain, United Kingdom and Thailand. He has published over 50 publications and received numerous awards. As an NIH-funded researcher, his whose inventions have led to over a dozen patent filings and a medical device startup company, Sonavex, which spun out of Johns Hopkins and has raised over 4 million dollars in funding. His basic science research focuses on tissue engineering and materials science for surgical applications as well as clinical outcomes research to improve both the delivery and results of transgender health care.
Question emailed from a reader:
“For Providers: What sort of issues do you run into the most when inputting and managing transgender patient data? Specifically, for the applications used to connect to insurers, manage medical records, bill claims, etc.”
I have mixed feelings about the idea of collecting SOGI info…while in theory it seems great to be able to provide information that would improve patient care, for myself, I would have questions about what they were going to do with the data, and where the electronic record might make itself known (for instance, with another provider that’s not so open-minded, maybe years down the road!). I don’t think I’d be in any shape to be carefully considering that kind of thing, either, when in an ER intake. Not that the initiative to change isn’t a great thing, but I’m surprised by the 90% willingness to provide SOGI information, because I’m definitely not alone in distrusting the medical system, especially when it comes to handling sensitive information or working with marginalized populations.